Because of the distance, our first scan wasn’t until about 16 weeks. That was when we found out that we were having twins. And it was a real shock! During scan they told us that they couldn’t find the membrane that normally separates the twins, but said not to stress about it. At the next scan, they still couldn’t find it and we realised then that actually it wasn’t there.
That was when everything went into turmoil. Because it was such a rare situation, no-one could give us accurate advice about exactly what this meant. Our twins were monochorionic, monoamniotic, so both shared the same fluid sac. We had an obstetrician in Hughenden, but she didn’t know much about it, so that was when we were moved over to the Townsville Hospital.
We started out with fortnightly scans, which meant me travelling 4 hours each way, in and out of Hughenden. I was still doing the school run each day, everything else as normal but travelling in every 2 weeks. Things plodded along, but they were underweight. As we did each scan it became clear that twin B wasn't gaining as much weight as twin A. At 24 weeks, my obstetrician was going to be away and he sent me to Brisbane for another specialist to take a look at how things were going.
When they scanned her there, they said it looked like she wasn’t going to make it. They said that we might have to intervene. We spoke to 4 or 5 different doctors and they all had their own different opinion, which made it really difficult. We just wanted to be told ‘This is what you need to do’ and we would do it.
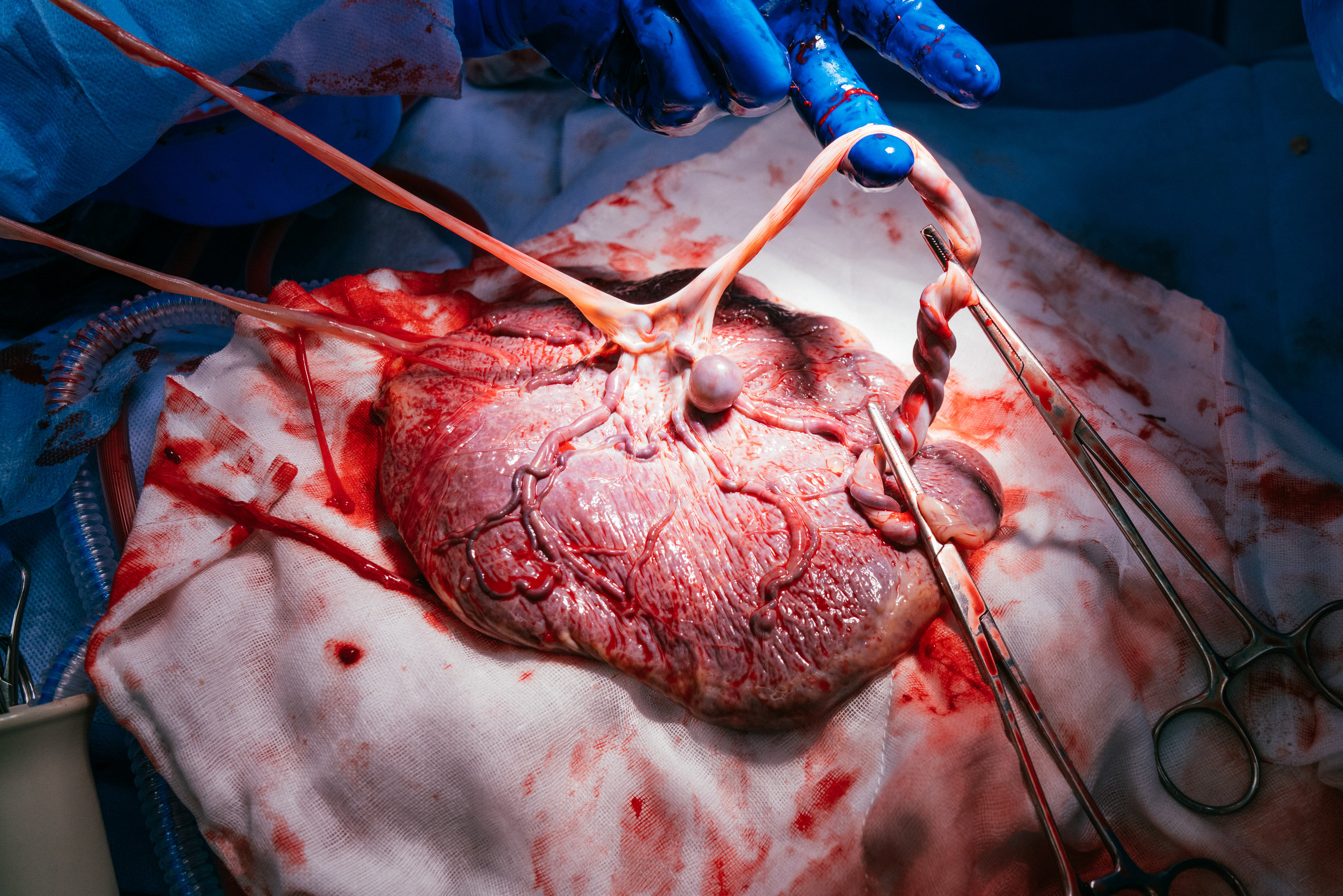
Because the babies' cords were only a short distance apart where they joined the placenta, they explained that it was like tree roots and the bigger roots were close together, making the chance of twin-to-twin transfusion syndrome a possibility. They were initially going to try and laser between the two, but because they were so close together, they couldn’t do that.
The other option they gave us was to clamp off twin B and let her die to save her sister. We didn’t want to make that decision, it still wasn’t definite that she couldn’t survive, so how could we possibly have the final word on that? We then spoke to another doctor who agreed with our decision to not to intervene if we didn’t have to. If twin A - the healthier one - dropped off, then we could make that decision. That was on the Friday. We then had had the weekend off, but when we went back in on Monday, we found that she had passed away.
In some ways it was better that way, because we didn’t have to make that decision ourselves. Of course it was incredibly sad, but it was in some way a relief, because it was nature's way, and God had made his decision.
So then what? The pregnancy remained high risk and we needed to keep monitoring. We went back to Townsville, started having weekly scans. I then became very anxious about it all - we knew their cords could still get entangled at any time without the membrane separating them, and our live baby could then die too. I requested daily monitoring, so we had it every day at the hospital to be sure she was OK and - eventually 10 weeks later - we had made it to 34 weeks. It was incredibly tiring and emotional - we just wanted to get to the end.
When we met Sophie, we were so relieved, so happy and blessed that she was healthy. I didn't know what to expect, I’d heard lots of stories about 34 week babies having breathing problems and other difficulties, but she’s just perfect. It was the biggest relief after everything that we'd been through.
We already had two girls names chosen, right from before my first son was born - Eleanor & Makayla. We had stuck with those names all the way through, but when we started having the dramas we decided that we just couldn’t name them. It was probably us trying to detach ourselves. I think it was a survival technique, we just put it off. Then in Brisbane before she passed away, without even talking about it we started calling our twin B Makayla. After she passed away, we went back to calling them twin A and twin B, I think again we just needed to distance ourselves from all that was going on.
When the girls were born, we decided we couldn’t take that name away from her. It was the name that she had when she was alive and when she passed, we couldn’t just take that name away. So she became Makayla Jayne. She received a care package from the hospital and inside, there was a little teddy bear that had the name Sophie on it. Sophie was another of the 4 girls names on our shortlist and we felt it was fitting that her sister had that name. Eleanor then became Sophie’s middle name and it all fell into place.
Makayla was baptised at the hospital - it took us a few days to bring ourselves to be able to do that. I didn’t see her until late on the day they were born, so with the surgery, it was still a bit of a blur. It was really important for us to have her baptised as a way of recognising that it really did happen, accepting, and letting go. We did it in the hospital room, with our family priest. It was really beautiful. We already had quite a few weeks after she passed to grieve, and we did a lot of that before she was born.
We were always very honest with the boys and when she passed we had to tell them straight away. My older son is quite intelligent so he had a million questions about where is she now, why is she still in there, how will they get her out, etc. It was really quite difficult because I had to deal with that as well as my own emotions. But he had to know, so we were honest and explained everything. Our youngest is quite an empathetic child and was very upset by it all. You would think he might not really understand, but even now says I miss my baby Makayla. On a level they can understand it.
My husband Tim has been my rock, he’s been so good. He gets emotional and that surprised me too, but he bottles it up a lot as well.
I still feel like I can’t quite breath easy just yet. When Sophie's out of hospital, then I’ll be on Cloud 9 I think. They say that she’ll be another 2 weeks if she puts on a good amount of weight and takes to the breastfeeding fully. We can’t wait to get her home.